Today was the start date for a federal policy that gives companies more leeway to skip insurance coverage for contraceptives. Companies can now limit coverage on moral or religious grounds -- so fewer women are likely to get coverage.
But the policy hasn't taken effect nationwide, because a federal judge blocked it in 13 states and Washington, D.C. -- a group that challenged it. In the Midwest, the policy is on hold in Illinois and Minnesota.
The Affordable Care Act requires most companies to offer health insurance that covers FDA-approved birth control at no cost, NPR noted. But the Trump administration developed rules making it easier for companies to avoid that requirement.
Sunday's ruling by U.S District Judge Haywood Gilliam in California raised questions about whether the new policy conflicts with the Affordable Care Act. The ruling also set up a longer court battle.
Gilliam also blocked the policy from taking effect in these states: California, Connecticut, Delaware, Hawaii, Maryland, New York, North Carolina, Rhode Island, Vermont, Virginia and Washington.
When the new rule was proposed in 2017, Roger Severino, an official with the U.S. Department of Health and Human Services, said it would affect only a small percentage of women.
But Dania Palanker, a preofessor at Georgetown University's Center on Health Insurance Reform, called it a "huge loophole" for employers, and predicted that a lot of women would be affected.
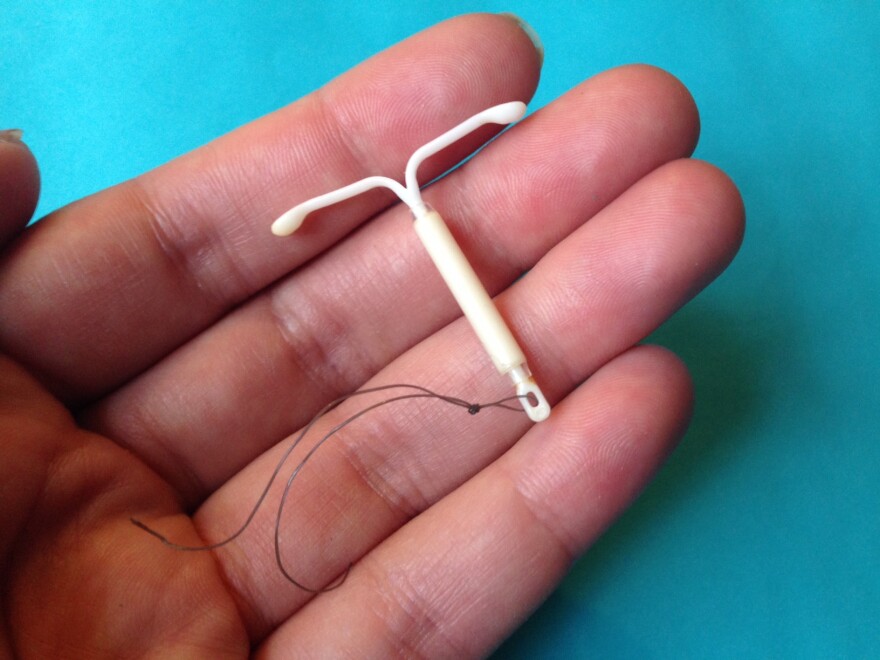
Women's right advocates said many employees would have to pay out of pocket for birth control pills -- which cost from $4 to more than $50 for a one-month supply -- or more than $1,000 for an intrauterine device.
Within weeks, the University of Notre Dame announced that it planned to stop providing birth control coverage to students and employees.
This story was produced by Side Effects Public Media, a news collaborative covering public health.